|
|
02 Features
Print To PDF
DisplayTitle Structure and Function of Dietary Fiber: The Physics of Fiber in the Gastrointestinal Tract
Authors Kyle J. Sloan1 and Johnson W. McRorie, Jr.2
Affiliations Procter & Gamble, Mason, OH, U.S.A.
1 Senior scientist, scientific communications, PharmD
2 Clinical scientist, PhD, FACG, AGAF, FACN
© 2020 Cereals & Grains Association
Abstract
CFWAbstract There are many misconceptions about the health benefits of “fiber” based on the misapplication of data generated on “dietary fiber” and “isolated fiber” sources to all fibers. The epidemiologic data on the benefits of dietary fiber lack the control necessary to determine whether it is the fiber or another aspect of a high-fiber diet that delivers a benefit. In contrast to dietary fiber, which is intrinsic and intact in foods, isolated fiber (e.g., fiber supplements) can be assessed for a direct effect on specific physiologic markers in well-controlled clinical trials. When isolated fibers have been studied, the metabolic benefits of lowering LDL cholesterol and improving glycemic control have been proven only for soluble gel-forming fibers like psyllium and beta-glucan. Gel-forming psyllium fiber has also been shown to provide a combination of satiety, energy intake reduction, and weight loss benefits. Some soluble nonviscous fermentable fructooligosaccharide (FOS) fibers have been shown to provide satiety benefits, but they have not been shown to provide all three benefits. In the large intestine, the delivery of a regularity benefit by fiber has also been challenged when the data from well-controlled trials is reviewed. There are only two mechanisms by which a fiber can provide a reduced constipation benefit, and both require that the fiber resist fermentation to arrive intact in stool: 1) a coarse insoluble fiber (e.g., coarse wheat bran) mechanically irritates the digestive mucosa; and 2) a viscous gel-forming fiber (e.g., psyllium) traps water in the gel, which resists dehydration throughout the large intestine. Psyllium is 3.4 times more effective than wheat bran for increasing stool output, making it the gold standard fiber for laxation. Only by recognizing that not all fibers are alike, can we identify the relevant properties to consider when choosing an isolated fiber for its specific proven health benefits.
Trying to reach content?
View Full Article
if you don't have access, become a member
Page Content The Institute of Medicine has published a definition of total fiber that differentiates “dietary fiber” (nondigestible carbohydrates and lignin that are intrinsic and intact in plants) from “functional fiber” (isolated, nondigestible carbohydrates that have been shown to have beneficial physiologic effects in humans) (1). Data supporting the health benefits of dietary fiber are derived from epidemiologic studies, which can be used to assess statistical associations but which lack the control necessary to establish causation. It is not possible, therefore, to separate the effects of an increase in dietary fiber intake from other aspects of a high-fiber diet, such as an increase in other biologically active nutrients or a decrease in fat intake. This is not a new concept. The National Academy of Sciences (2) published a report 20 years ago that states, “There is no conclusive evidence that it is dietary fiber rather than the other components of vegetables, fruits, and cereal products that reduces the risk of those diseases.” Even though causation cannot be established, the recommended adequate intake for fiber (14 g/1,000 kcal) is based on epidemiologic data: the median fiber intake that is associated with the lowest risk of coronary heart disease (1). Based on average calorie intake, this translates to a recommended dietary fiber intake of 25 g/day for adult women and 38 g/day for adult men. In contrast to these recommendations, average dietary fiber intake for U.S. adults is only about 15 g/day.
In contrast to dietary fiber, “isolated fibers” can be directly assessed for beneficial physiological effects in randomized, well-controlled clinical studies. By definition, an isolated fiber must show clinical evidence of a health benefit to be considered a functional fiber. The term “fiber supplement” may actually be misleading to health-care professionals and consumers because it implies that regular consumption will bridge the “fiber gap” between recommended adequate intakes and average intake by individuals and provide the health benefits associated with a high-fiber diet. For most fiber supplements, however, this assertion is not supported by reproducible, well-controlled clinical evidence of a cardiovascular benefit. The following sections provide an overview of the physical effects of fiber in the gut and how these physical effects translate into specific health benefits. An understanding of the physical effects required to provide specific health benefits will help debunk enduring misconceptions about the health benefits of fiber supplements.
Types of Isolated Fiber and Where and How They Work
Isolated fibers (e.g., fiber supplements) can be divided into insoluble fiber (remains as discrete particles in water) and soluble fiber (dissolves in water). Soluble fibers can be subdivided into nonviscous (e.g., inulin, partially hydrolyzed guar gum [PHGG]), viscous (e.g., methylcellulose), and viscous gel-forming (e.g., psyllium, beta-glucan, raw guar gum). Metabolic benefits, including cholesterol lowering, improved glycemic control, and satiety and weight loss, are a function of viscous gel-forming fibers in the small intestine. Regularity and reduced constipation is a function of the physical effects of fiber in the large intestine.
Small Intestine and Metabolic Health Benefits. Metabolic health benefits are a function of fiber viscosity in the small intestine (3). Insoluble fibers do not provide metabolic health benefits and have been used as a placebo in clinical studies. Although it is true that soluble fibers can provide metabolic health benefits, it is not true that all soluble fibers provide these benefits. Clinical data show that only gel-forming fibers (e.g., psyllium, beta-glucan) are sufficiently viscous to significantly lower elevated serum cholesterol and fasting blood glucose and provide a satiety and weight loss benefit (3). Nonviscous fibers (e.g., wheat dextrin, PHGG) and viscous fibers (e.g., methylcellulose) do not provide metabolic health benefits (3).
Cholesterol Lowering. The primary mechanism by which a gel-forming fiber lowers elevated serum cholesterol is by trapping and eliminating bile acids (4). Bile is produced by the liver, stored and concentrated in the gall bladder, and released into the small bowel in response to a meal. Bile facilitates the digestion and absorption of dietary lipids and is so highly conserved that it can be recycled several times within a given meal. In contrast to nutrient absorption, which can occur along the entire 7 m length of the small bowel, the recovery of bile is limited to the terminal ileum, providing only a brief opportunity for active uptake. A gel-forming fiber becomes more concentrated as water is reabsorbed along the length of the small intestine, which increases viscosity and interferes with exposure of bile to the mucosa for active uptake. The trapped bile is eliminated via the stool. This reduction in the bile acid pool causes hepatocytes to compensate by expressing LDL receptors. This increases LDL (“bad”) cholesterol clearance from the blood in order to synthesize more bile acids (cholesterol is a component of bile). The clearance of LDL cholesterol from the blood effectively lowers serum LDL cholesterol and total cholesterol concentrations, without significantly affecting HDL (“healthy”) cholesterol. Only gel-forming fiber supplements (e.g., psyllium, high molecular weight beta-glucan), when consumed with meals to coincide with bile release, have the requisite high viscosity to effectively lower elevated serum cholesterol concentrations (5). Nonviscous fibers (e.g., wheat dextrin, PHGG) and non–gel-forming viscous fibers (e.g., methylcellulose) have no significant effect on cholesterol lowering (5).
The importance of viscosity was demonstrated in a study of beta-glucan. In this double-blind, parallel-design, multicenter clinical study, 386 subjects were randomly assigned to receive cereal containing insoluble wheat bran (negative control) or one of three gel-forming oat bran cereals (3–4 g/day of beta-glucan that was high, medium, or low viscosity) (6). The degree of processing (heat and pressure for extrusion) was used to lower the normally high viscosity of gel-forming beta-glucan. The study showed that cholesterol lowering was highly correlated with the viscosity of the gel-forming fiber: the high-viscosity beta-glucan had the greatest effect on serum cholesterol, the low-viscosity beta-glucan had no significant effect, and the effect of the medium-viscosity beta-glucan was in between. Two challenges are encountered with beta-glucan—concentration (there are only 2 g of beta-glucan in a cup of oatmeal) and fermentation—both of which limit the dose per day. In contrast, a teaspoon of a psyllium fiber supplement contains 3.4 g of nonfermented psyllium fiber.
A review of the effectiveness of psyllium fiber for lowering elevated serum cholesterol included 21 randomized, well-controlled clinical studies (more than 1,500 subjects) at doses of 6–15 g/day (most studies at 10 g/day). All studies showed a statistically significant cholesterol-lowering effect, with reductions ranging from 6 to 24% for LDL cholesterol versus placebo (3). The efficacy of psyllium fiber tended to be greatest in studies assessing patients with a high baseline cholesterol concentration and in studies where the diet was not restricted. A recent meta-analysis of 28 studies (n = 1,924) confirmed the review, showing that psyllium fiber (mean dose of 10.2 g/day) reduced LDL cholesterol by 13 mg/dL (7). In addition, the cholesterol-lowering benefit for psyllium fiber is additive to the effects of statin drugs (8). A recent meta-analysis showed a clinically and statistically significant (P = 0.001) cholesterol-lowering advantage for psyllium fiber plus statin combination treatment over a statin alone. Adding psyllium fiber resulted in reductions in LDL cholesterol equivalent to doubling the statin dose. The authors concluded that the data suggest psyllium fiber taken before meals adds to the efficacy of statins, providing an easy to implement dietary intervention for those who cannot tolerate the side effects associated with higher-dose statins (8). Raw guar gum is another viscous gel-forming fiber, but it gels so rapidly that it is not palatable. Products marketed in the United States hydrolyze guar gum until it is nonviscous (PHGG), improving palatability but eliminating the cholesterol-lowering effect.
In summary, cholesterol-lowering efficacy is highly correlated with the viscosity of the hydrated fiber, and only gel-forming fibers (e.g., psyllium, beta-glucan) are sufficiently viscous to effectively lower elevated serum cholesterol. Psyllium and beta-glucan are the only isolated fibers that have been approved by the U.S. Food and Drug Administration (FDA) to claim a reduced risk of cardiovascular disease by lowering serum cholesterol. Because the adequate intake recommendations for fiber are based on a reduced risk of cardiovascular disease, it is reasonable to assert that only those fibers that are approved by the FDA to claim a reduced risk of cardiovascular disease (i.e., psyllium and beta-glucan) (9) should be recommended to bridge the fiber gap in dietary fiber intake.
Improved Glycemic Control. As with cholesterol lowering, improved glycemic control is a viscosity, gel-dependent phenomenon. More than four decades ago it was clearly demonstrated that the glycemic effects of soluble fiber are proportional to the viscosity of the hydrated fiber (10). In this postprandial study, volunteers consumed 50 g of liquid glucose with and without added fiber. Gel-forming raw guar gum exhibited a clinically meaningful decrease in postprandial blood glucose compared with liquid glucose alone. This beneficial effect was abolished, however, when the guar gum was hydrolyzed to the nonviscous form (PHGG) that is marketed today. After comparing several fibers with different viscosities, the authors concluded that the reduction in postprandial blood glucose level had a nearly perfect correlation with the viscosity of the hydrated fiber (r = 0.926; P < 0.01) (10). Although postprandial glucose studies are a useful tool for assessing acute glycemic effects, long-term (multimonth) data from well-controlled intervention clinical studies are necessary to establish a clinically meaningful health benefit for improved glycemic control.
Several multimonth clinical studies have demonstrated that consumption of a soluble, viscous gel-forming fiber (e.g., psyllium), when dosed with meals, can lower elevated fasting blood glucose and HbA1c in subjects at risk for developing type 2 diabetes and patients being treated for type 2 diabetes (11). The long-term glycemic effects of psyllium fiber were proportionate to baseline glycemic control: no significant effect in euglycemia, a modest effect in prediabetes and metabolic syndrome, and a marked effect in type 2 diabetes. The primary mechanism for improving glycemic control is a significant increase in the viscosity of chyme, which slows the interactions of digestive enzymes and nutrients in the small intestine. This slows the degradation of complex nutrients into absorbable components and slows the absorption of glucose and other nutrients at the mucosal brush border. Nutrients are normally absorbed early in the small intestine, but an increase in viscosity and subsequent slowing of nutrient degradation and absorption leads to increased delivery of nutrients to more distal regions of the small intestine (e.g., distal ileum), where they are not normally present. Nutrients arriving in the distal ileum can stimulate mucosal L-cells to release glucagon-like peptide-1 (GLP-1) into the bloodstream. GLP-1 significantly decreases appetite, increases beta-cell growth (cells that produce insulin), improves insulin production and sensitivity, and decreases glucagon secretion (a peptide that stimulates glucose production in the liver) (5). It is important to note that although a viscous fiber can slow the absorption of nutrients, it does not reduce total nutrient absorption. Unlike bile, which is only absorbed in a short segment of the distal ileum, nutrients are absorbed along the entire 7 m length of the small intestine (approximately equal to the area of a tennis court), providing ample opportunity for nutrient absorption to occur (3).
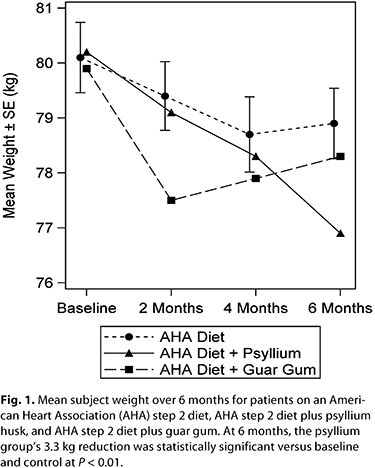 Satiety, Energy Intake, and Weight Loss. One of the goals of a high-fiber diet is long-term weight loss and maintenance. There is a hierarchy of data: increased satiety (decreased hunger) is a feeling that may be predictive of decreased energy intake; decreased energy intake may be predictive of short-term weight loss; short-term weight loss may be predictive of long-term weight loss and maintenance. Nonviscous soluble fibers, such as synthetic wheat dextrin, have no effect on satiety (12–14). Studies that only assess satiety may be misleading, in that some fibers (e.g., fructooligosaccharides [FOS]) have shown a satiety effect, while in the same study showing no effect on energy intake (15). Because satiety is lower in the hierarchy than energy intake, data showing no effect on energy intake means that the satiety effect is not predictive and must be disregarded. In the absence of contradictory higher order data, lower order data should be considered valid. In contrast to nonviscous fibers, viscous gel-forming fibers can have a significant effect on satiety and hunger, energy intake, and weight loss (16). Psyllium is a viscous gel-forming fiber that has been shown to have significant effects on satiety and hunger (17), energy intake (19% reduction) (18), and weight loss (18–20). In one 6 month study, readily fermented guar gum (7 g/day) showed initial weight loss followed by weight regain, while nonfermented psyllium fiber (7 g/day) showed steady weight loss across all time points (at 6 months: ‑3.3 kg versus baseline and ‑2.1 kg versus diet alone; P < 0.01) (20) (Fig. 1). Satiety, Energy Intake, and Weight Loss. One of the goals of a high-fiber diet is long-term weight loss and maintenance. There is a hierarchy of data: increased satiety (decreased hunger) is a feeling that may be predictive of decreased energy intake; decreased energy intake may be predictive of short-term weight loss; short-term weight loss may be predictive of long-term weight loss and maintenance. Nonviscous soluble fibers, such as synthetic wheat dextrin, have no effect on satiety (12–14). Studies that only assess satiety may be misleading, in that some fibers (e.g., fructooligosaccharides [FOS]) have shown a satiety effect, while in the same study showing no effect on energy intake (15). Because satiety is lower in the hierarchy than energy intake, data showing no effect on energy intake means that the satiety effect is not predictive and must be disregarded. In the absence of contradictory higher order data, lower order data should be considered valid. In contrast to nonviscous fibers, viscous gel-forming fibers can have a significant effect on satiety and hunger, energy intake, and weight loss (16). Psyllium is a viscous gel-forming fiber that has been shown to have significant effects on satiety and hunger (17), energy intake (19% reduction) (18), and weight loss (18–20). In one 6 month study, readily fermented guar gum (7 g/day) showed initial weight loss followed by weight regain, while nonfermented psyllium fiber (7 g/day) showed steady weight loss across all time points (at 6 months: ‑3.3 kg versus baseline and ‑2.1 kg versus diet alone; P < 0.01) (20) (Fig. 1).
Large Intestine Effects: It’s All about the Water. Regularity can be defined as the regular (e.g., daily) elimination of bulky, soft, easy-to-pass stools. Constipation can be defined as infrequent bowel movements (BMs) (<3 BMs/week) and elimination of small, hard, difficult-to-pass stools. Normal BM frequency ranges from 3 BMs/week to 3 BMs/day. Although BM frequency is often used as a measure of regularity, it can be misleading and should not be the primary measure. For example, if a person strains to pass a single small or hard marble-like stool 4 days/week, and another person has normal stools without straining 2.5 days/week, the individual with the higher BM frequency is constipated, while the individual with the lower BM frequency is not. In the context of fiber consumption, the most important considerations for assessing a clinically meaningful benefit for constipation are evidence of a significant increase in stool output (g/day in healthy individuals and g/week in constipated individuals) and stool water content (%). To treat constipation, an effective fiber must provide a mechanism that increases water in the large intestine, which will increase both stool output (stool is mostly water) and will soften hard stool by increasing stool water content (21). The water content of stool is inversely proportional to stool viscosity (22). As stool water content decreases, stool viscosity increases exponentially, so that a small change in water content (e.g., 2%) results in a large change in stool consistency: hard stool is <72% water, formed stool is ~74% water, and soft stool ~76% water. By increasing stool water content, an effective fiber therapy can soften hard stool and significantly increase stool output—both of which make stools easier to pass without straining.
There are only two mechanisms by which a fiber can increase stool water content and provide a significant laxative effect: 1) large coarse insoluble fiber particles (e.g., coarse wheat bran) mechanically irritate the mucosa of the large bowel, stimulating mucous and water secretion; and 2) the high water-holding capacity of soluble viscous gel-forming fiber (e.g., psyllium) resists dehydration throughout the large intestine (5). For both mechanisms, the fiber must resist fermentation and remain intact throughout the large intestine (it must be present in stool; a prerequisite for the first mechanism) and must increase stool water content (a prerequisite for the second mechanism), leading to bulky, soft stools that are easy to pass. It is a common misconception that all fiber provides a regularity benefit (21). Most epidemiologic studies do not support a statistical association between a high-fiber diet and a decreased risk of constipation or a low-fiber diet and an increased risk of constipation (23–27). When studied in isolation, fermentable fibers (e.g., inulin, FOS, PHGG) are not different from placebo for stool output or consistency (3,21). A meta-analysis (28) has been cited as evidence that prebiotics have a regularity benefit, but on close inspection it was psyllium (P < 0.000001) that drove the fiber effect in the meta-analysis, while wheat bran (P = 0.19) and prebiotics (P = 0.41) had no significant effect. Further, some isolated fibers can actually have a stool-hardening effect (e.g., wheat dextrin, fine wheat bran) by adding only to the dry mass of stool, which can be constipating (4).
In summary, dietary fiber and most isolated fibers are not effective for improving regularity, and some can be constipating. Therefore, a generic recommendation to “increase fiber intake” is akin to a recommendation to “increase pill intake” without regard to therapeutic benefit or side effects. Any recommendation for treatment or prevention of constipation should be based on the totality of the clinical evidence.
For more than three decades, wheat bran has been incorrectly touted as the “gold standard” fiber for regularity (29). The assertion was based on a table in a book chapter that shows that wheat bran had a higher stool output per gram of fiber consumed (g of stool/g of fiber [g/g]) (30). On close inspection, however, a footnote below the table states that wheat bran was only 44% fiber. This reduced the reported stool output (5.4 g/day) to less than half (5.4 g/g × 0.44 = 2.4 g/g), making psyllium (85% fiber) the true gold standard (4.0 g/g × 0.85 = 3.4 g/g). This was confirmed by a recent comprehensive review and meta-analysis that shows psyllium was 3.4 times more effective than wheat bran for increasing stool output in patients with constipation (31). Both psyllium and coarse wheat bran increased stool water content, a stool softening effect, while finely ground wheat bran added only to the dry mass of stool and decreased stool water content, a stool-hardening effect. Unfortunately, wheat bran food labels do not provide information on coarse versus fine wheat bran, so there is no way to predict efficacy at the point of purchase. The review also shows that psyllium was equally effective in healthy subjects and patients with chronic constipation, while wheat bran was much less efficacious for patients with constipation. Thus, studies showing efficacy in healthy subjects may not be predictive of efficacy in subjects with constipation and should be viewed with caution (31).
Misconceptions about Dietary Fiber and Isolated Fibers
There are numerous misconceptions about fiber in the published literature and online. A few examples are summarized below.
“All Fiber Is Good for You.” As discussed earlier, the benefits associated with a high-fiber diet may not actually be due to the fiber per se, but may instead be due to other health-promoting components of a high-fiber diet (e.g., micronutrients, low fat intake). Most isolated fibers (e.g., nonviscous fibers) have no placebo-controlled clinical evidence of efficacy for cholesterol lowering, improved glycemic control, satiety and weight loss, or regularity. Further, some fibers (e.g., wheat dextrin, fine wheat bran) can actually be constipating. Not all fibers are the same, and care must be taken when recommending fiber to only consider those with clinically proven health benefits (Table I).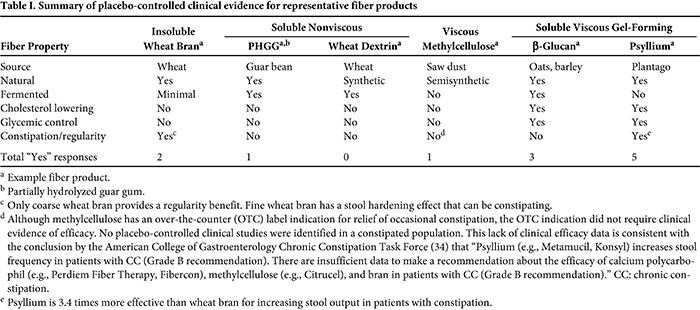
“Any Isolated Fiber Can Bridge the Fiber Gap.” The fiber gap is the difference between the recommended adequate intake level of dietary fiber (e.g., in the United States, 25 g/day for adult women and 38 g/day for adult men) minus actual intake of dietary fiber (e.g., 15 g/day). In this example the fiber gap would be 10 g/day for adult women and 23 g/day for adult men. It is important to recognize that the adequate intake level for fiber (14 g/1,000 kcal) is based on epidemiologic data: the median fiber intake associated with the lowest risk of coronary heart disease (1). Therefore, to bridge the defined fiber gap , only those fibers that are approved by the FDA to claim a reduced risk of coronary heart disease by reducing serum cholesterol (i.e., psyllium and beta-glucan) (9) are qualified. A nonviscous fiber product with a claim that it “helps bridge the fiber gap” misleads consumers.
Generic and Specific Recommendations. Generic recommendations to “increase fiber intake” and specific recommendations for isolated fibers with no clinical evidence of efficacy in treating constipation have been published in patient information pages on constipation (32,33). As discussed earlier, most isolated fibers have no laxative effect, at least two (fine wheat bran and wheat dextrin) can be constipating, and most epidemiologic studies show no association between dietary fiber intake and the incidence of constipation (3,4). This lack of data supporting clinical efficacy is consistent with the conclusion by the American College of Gastroenterology Chronic Constipation Task Force (34) (CC = chronic constipation) that “Psyllium (e.g., Metamucil, Konsyl) increases stool frequency in patients with CC (Grade B recommendation). There are insufficient data to make a recommendation about the efficacy of calcium polycarbophil (e.g., Perdiem Fiber Therapy, Fibercon), methylcellulose (e.g., Citrucel), and bran in patients with CC (Grade B recommendation).” Treatment guidelines for constipation should make specific, evidence-based recommendations as they pertain to fiber.
“In Vitro Fermentation Data Are Predictive of the Human Experience.” In vitro (benchtop and test tube) data are intended to generate hypotheses that then can be tested in clinical studies. If the clinical data do not support the in vitro hypothesis, then the in vitro results are not predictive of the human experience and should be disregarded. Such is the case for in vitro data comparing the fermentation of methylcellulose and psyllium (35). The study showed that methylcellulose was rapidly fermented (up to 76% “disappeared” at 12 hr), while psyllium was minimally fermented (up to 8% disappeared at 12 hr). Psyllium showed a slight increase in carbon dioxide in vitro. It should be noted, however, that carbon dioxide is produced by every living cell in the human body and is rapidly absorbed into the blood stream or exhaled without increasing intestinal gas or flatulence. It should also be noted that in vitro testing requires that psyllium in solution remains a low-viscosity, readily stirred liquid, which requires using a low concentration of psyllium that prevents gel formation. It is this three-dimensional gel that prevents fermentation in the human gastrointestinal tract (36). Five placebo-controlled clinical studies showed that psyllium was not fermented in the human gastrointestinal tract and did not increase flatulence (37–41). Methylcellulose also showed no evidence of fermentation in the human gastrointestinal tract (39,40), in contrast to rapid fermentation in vitro (35). The in vitro data, therefore, are not predictive of the human experience and must be disregarded.
Summary
All fibers are not alike. Only viscous gel-forming fibers (e.g., psyllium, beta-glucan) have a significant effect on cholesterol lowering, improved glycemic control, and satiety and weight loss. Nonviscous soluble fibers (e.g., wheat dextrin, PHGG) do not provide these health benefits. There are only two mechanisms by which a fiber effect can provide a regularity or reduced constipation benefit, and both require that the fiber resist fermentation and arrive intact in stool: 1) coarse insoluble fiber (e.g., coarse wheat bran) mechanically irritates the gut mucosa, stimulating secretion of water and mucous; and 2) viscous gel-forming fiber (i.e., psyllium) resists dehydration throughout the large intestine by trapping water in the gel. Both mechanisms increase stool water content, which increases stool bulk and softens stool. Psyllium is 3.4 times more effective than wheat bran for increasing stool output, making it the gold standard fiber for laxation. Fermented soluble fibers (e.g., PHGG, inulin) do not provide a regularity benefit, and some fibers (e.g., wheat dextrin, fine wheat bran) have a stool-hardening effect that can be constipating. Making a generic recommendation to increase fiber intake would be akin to making a recommendation to increase pill intake without regard to therapeutic benefit. Any recommendation to increase fiber intake should be specific to the desired health benefit and specific to the isolated fiber that is clinically proven to provide that health benefit.
References References
- Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes: Energy, Carbohydrates, Fiber, Fat, Fatty Acids Cholesterol, Protein and Amino Acids. National Academies Press, Washington, DC, 2002.
- National Research Council. Recommended Dietary Allowances, 10th ed. National Academies Press, Washington, DC, 1989.
- McRorie, J., and McKeown, N. An evidence-based approach to resolving enduring misconceptions about insoluble and soluble fiber—Understanding the physics of functional fibers in the gastrointestinal tract. J. Acad. Nutr. Diet. 117:251, 2017.
- Lambeau, K., and McRorie, J. Fiber supplements and clinically proven health benefits: How to recognize and recommend an effective fiber therapy. J. Am. Assoc. Nurse Pract. 29:216, 2017.
- McRorie, J., and Fahey, G. Fiber supplements and clinically meaningful health benefits: Identifying the physiochemical characteristics of fiber that drive specific physiologic effects. Page 161 in: The CRC Handbook on Dietary Supplements in Health Promotion. T. C. Wallace, ed. CRC Press, Florence, KY, 2015.
- Wolever, T., Tosh, S., Gibbs, A., and Brand-Miller, J. Physicochemical properties of oat beta-glucan influence its ability to reduce serum LDL cholesterol in humans: A randomized clinical trial. Am. J. Clin. Nutr. 92:723, 2010.
- Jovanovski, E., Yashpal, S., Komishon, A., Zurbau, A., Mejia, S., Ho, H., Li, D., Sievenpiper, J., Duvnjak, L., and Vuksan, V. Effect of psyllium (Plantago ovata) fiber on LDL cholesterol and alternative lipid targets, non-HDL cholesterol and apolipoprotein B: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 108:922, 2018.
- Brum, J., Ramsey, D., McRorie, J., Bauer, B., and Kopecky, S. Meta-analysis of usefulness of psyllium fiber as adjuvant anti-lipid therapy to enhance cholesterol lowering efficacy of statins. Am. J. Cardiol. 122:1169, 2018.
- U.S. Food and Drug Administration. Authorized health claims that meet the Significant Scientific Agreement (SSA) standard. Published online at www.fda.gov/food/food-labeling-nutrition/authorized-health-claims-meet-significant-scientific-agreement-ssa-standard. FDA, Silver Spring, MD, 2018.
- Jenkins, D., Wolever, T., Leeds, A., Gassull, M., Haisman, P., and Dilawari, J. Dietary fibres, fibre analogues, and glucose tolerance: Importance of viscosity. BMJ 1:1392, 1978.
- Gibb, R., McRorie, J., Russell, D., Hasselblad, V., and D’Alessio, D. Psyllium fiber improves glycemic control proportional to loss of glycemic control: A meta-analysis of data in euglycemic subjects, patients at risk of type 2 diabetes mellitus, and patients being treated for type 2 diabetes mellitus. Am. J. Clin. Nutr. 102:1604, 2015.
- 12. van den Heuvel, E., Wils, D., Pasman, W., Saniez, M., and Kardinaal, A. Dietary supplementation of different doses of NUTRIOSE-FB, a fermentable dextrin, alters the activity of faecal enzymes in healthy men. Eur. J. Nutr. 44:445, 2005.
- van den Heuvel, E., Wils, D., Pasman, W., Bakker, M., Saniez, M., and Kardinaal, A. Short-term digestive tolerance of different doses of NUTRIOSE FB, a food dextrin, in adult men. Eur. J. Clin. Nutr. 58:1046, 2004.
- Pasman, W., Wils, D., Saniez, M., and Kardinaal, A. Long-term gastrointestinal tolerance of NUTRIOSE FB in healthy men. Eur. J. Clin. Nutr. 60:1024, 2006.
- de Luis, D., de la Fuente, B., Izaola, O., Aller, R., Gutiérrez, S., and Morillo, M. Double blind randomized clinical trial controlled by placebo with a FOS enriched cookie on satiety and cardiovascular risk factors in obese patients. Nutr. Hosp. 28:78, 2013.
- Slavin, J. Position of the American Dietetic Association: Health implications of dietary fiber. J. Am. Diet. Assoc. 108:1716, 2008.
- Brum, J., Gibb, R., Peters, J., and Mattes, R. Satiety effects of psyllium in healthy volunteers. Appetite 105:27, 2016.
- Pal, S., Ho, S., Gahler, R. J., and Wood, S. Effect on insulin, glucose and lipids in overweight/obese Australian adults of 12 months consumption of two different fibre supplements in a randomised trial. Nutrients 9:91, 2017.
- Pal, S., Khossousi, A., Binns, C., Dhaliwal, S., and Ellis, V. The effect of a fibre supplement compared to a healthy diet on body composition, lipids, glucose, insulin and other metabolic syndrome risk factors in overweight and obese individuals. Br. J. Nutr. 105:90, 2011.
- Cicero, A., Derosa, G., Bove, M., Imola, F., Borghi, C., and Gaddi, A. Psyllium improves dyslipidaemia, hyperglycaemia and hypertension, while guar gum reduces body weight more rapidly in patients affected by metabolic syndrome following an AHA step 2 diet. Mediterr. J. Nutr. Metab. 3:47, 2010.
- McRorie, J., and Chey, W. Fermented fiber supplements are no better than placebo for a laxative effect. Dig. Dis. Sci. 61:3140, 2016.
- McRorie, J., Daggy, B., Morel, J., Diersing, P., Miner, P., and Robinson, M. Psyllium is superior to docusate sodium for treatment of chronic constipation. Aliment. Pharmacol. Ther. 12:491, 1998.
- Dukas, L., Willett, W., and Giovannucci, E. Association between physical activity, fiber intake, and other lifestyle variables and constipation in a study of women. Am. J. Gastroenterol. 98:1790, 2003.
- Markland, A., Palsson, O., Goode, P., Burgio, K., Busby-Whitehead, J., and Whitehead, W. Association of low dietary intake of fiber and liquids with constipation: Evidence from the national health and nutrition examination survey. Am. J. Gastroenterol. 108:796, 2013.
- Campbell, A., Busby, W., and Horwath, C. Factors associated with constipation in a community-based sample of people aged 70 years and over. J. Epidemiol. Community Health 47:23, 1993.
- Whitehead, W., Drinkwater, D., Cheskin, L., Heller, B., and Schuster, M. Constipation in the elderly living at home. Definition, prevalence, and relationship to lifestyle and health status. J. Am. Geriatr. Soc. 37:423, 1989.
- Everhart, J., Go, V., Johannes, R., Fitzsimmons, S., Roth, H., and White, L. A longitudinal survey of self-reported bowel habits in the United States. Dig. Dis. Sci. 34:1153, 1989.
- Christodoulides, S., Dimidi, E., Fragkos, K., Farmer, A., Whelan, K., and Scott, S. Systematic review with meta-analysis: Effect of fibre supplementation on chronic idiopathic constipation in adults. Aliment. Pharmacol. Ther. 44:103, 2016.
- Slavin, J. Fiber and prebiotics: Mechanisms and health benefits. Nutrients 5:1417, 2013.
- Cummings, J. H. The effect of dietary fiber on fecal weight and composition. In: CRC Handbook of Dietary Fiber in Human Nutrition, 3rd ed. G. A. Spiller, ed. CRC Press, Boca Raton, FL, 2001.
- McRorie, J., Fahey, G., Gibb, R., and Chey, W. Laxative effects of wheat bran and psyllium: Resolving enduring misconceptions about fiber in treatment guidelines for chronic idiopathic constipation. J. Am. Assoc. Nurse Pract. 32:15, 2020.
- American Association of Family Practitioners. Information from your family doctor: Constipation. Am. Fam. Phys. 82:1440, 2010.
- Wald, A. JAMA patient page. Constipation. J. Am. Med. Assoc. 315:214, 2016.
- Ford, A. C., Moayyedi, P., Lacy, B. E., Lembo, A. J., Saito, Y. A., Schiller, L. R., Soffer, E. E., Spiegel, B. M., Quigley, E. M., and Task Force on the Management of Functional Bowel Disorders. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am. J. Gastroenterol. 109:S2, 2014.
- Campbell, J., and Fahey, G. Psyllium and methylcellulose fermentation properties in relation to insoluble and soluble fiber standards. Nutr. Res. 17:619, 1997.
- Marlett, J., and Fischer, M. The active fraction of psyllium seed husk. Proc. Nutr. Soc. 62:207, 2003.
- Marlett, J., Li, B., Patrow, C., and Bass, P. Comparative laxation of psyllium with and without senna in an ambulatory constipated population. Am. J. Gastroenterol. 82:333, 1987.
- Marteau, P., Flourie, B., Cherbut, C., Correze, J., Pellier, P., Seylaz, J., and Rambaud, J. Digestibility and bulking effect of ispaghula husks in healthy humans. Gut 35:1747, 1994.
- Zumarraga, L., Levitt, M., and Suarez, F. Absence of gaseous symptoms during ingestion of commercial fibre preparations. Aliment. Pharmacol. Ther. 11:1067, 1997.
- Levitt, M., Furne, J., and Olsson, S. The relation of passage of gas and abdominal bloating to colonic gas production. Ann. Intern. Med. 24:422, 1996.
- Wolever, T., Wa, P., Spadafora, P., and Robb, P. Guar, but not psyllium, increases breath methane and serum acetate concentrations in human subjects. Am. J. Clin. Nutr. 55:719, 1992.
|